The Most (and Least) Sleep-Deprived U.S. Cities
Which major cities across the U.S. aren’t getting enough quality rest?

In 2020, nearly 15% of American adults reported trouble falling asleep, and about 18% had difficulty staying asleep.1 And those are the percentages of us who are aware of the problem. Not getting enough sleep is called sleep deprivation, and it can have a major impact on your quality of life. Besides impacting your ability to focus and function at work or school, a lack of sleep has been linked to chronic health conditions like heart disease, kidney disease, diabetes, high blood pressure, stroke, and others.2
We conducted a study on the 100 most populous U.S. cities using primarily CDC data, divided the information into weighted categories, graded each state’s sleep duration and quality, and then ranked each city from most to least sleep-deprived.
Jump to:
Key takeaways
- Both Norfolk, Virginia, and New Orleans, Louisiana — the top two most sleep-deprived cities — ranked high for short sleep duration and poor sleep quality.
- Nearly all of the ten most sleep-deprived cities are in the eastern half of the U.S.
- Wake up, Ohioans! (Er, actually, don’t.) Ohio is the only state with multiple cities on the top ten most sleep-deprived list — including Toledo (4th), Cincinnati (5th), and Cleveland (9th).
- Both California and Minnesota have multiple cities among the ten least sleep-deprived locations.
Sleep-deprived cities: an overview
May is “Better Sleep Month,” a time to acknowledge the fundamentally important role of sleep in our health.2 To recognize this, our research team developed a study to find out which major cities across the United States appear to be suffering the most from sleep deprivation. Using federal data from sources like the CDC’s Behavioral Risk Factor Surveillance System and its Population Level Analysis and Community Estimates (PLACES) databases, we combined six weighted metrics to create a ranking system that scores each city’s average sleep duration and sleep quality.
While sleep duration data is relatively straightforward and the subject of more widespread attention, it doesn’t paint a full picture of sleep deprivation. To be more comprehensive, we took five distinct factors into account in order to paint a picture of sleep quality for each city. Those five factors that significantly contribute to poor sleep quality include the prevalence of the following:
Leisure-time physical activity
Research shows that getting regular exercise can improve your sleep quality. A 2023 review of studies examining the relationship between physical activity and sleep found that regular, moderate-intensity exercise can reduce how long it takes to fall asleep and alleviate the symptoms of sleep disorders, like insomnia, daytime sleepiness, and sleep apnea.3
The review authors explain that this positive effect on sleep can be attributed to physical activity increasing the production of melatonin, reducing stress, improving mood, and promoting proper body temperature regulation.3
Obesity
While several factors can contribute to obstructive sleep apnea, obesity is “one of the main components,” according to the authors of a 2018 review.4 Sleep apnea can lead to waking up repeatedly throughout the night, daytime fatigue, nighttime restlessness, and other symptoms that impact your sleep quality.5 But sleep apnea isn’t the only thing linking obesity and sleep.
As explained by Yale Medicine endocrinologist Dr. Brian Wojeck, MD, MPH, “Sleep deprivation can create an imbalance in the hormones that regulate your appetite — ghrelin and leptin. Leptin helps you feel full; ghrelin makes you feel hungry. Leptin levels typically rise during sleep, so if you aren’t getting enough sleep, your leptin levels decrease, so you feel hungrier and are, therefore, likelier to eat excessively and gain weight.”6 This means that, in a way, obesity and poor sleep can worsen each other.
High alcohol consumption
Though drinking alcohol can momentarily increase feelings of relaxation and sleepiness, studies show that it actually leads to more frequent awakenings during the night and early morning. Research indicates that those who consume excessive amounts of alcohol tend to suffer from poor sleep quality, and those with alcohol use disorders often report insomnia.7
Additionally, according to the results of a 2018 review, higher levels of alcohol consumption increase the risk of developing obstructive sleep apnea by 25% on average.8
Mental distress
If you’ve ever found yourself lying awake in bed after a long and stressful day, then you’re well aware of the impact mental distress can have on your sleep. Feelings of stress and anxiety increase agitation, arousal, and alertness, all of which make it difficult to get a good night’s rest.9
People under frequent stress often report issues sleeping, and trouble sleeping can lead to or exacerbate psychological problems. For example, an older study from 2007 on over 10,000 adults found that chronic insomnia increases the risk of developing depression or anxiety.10 And with concerns like insomnia and nightmares frequently reported by those with anxiety disorders, and 75% of people with depression reporting trouble falling asleep or staying asleep, it’s easy to see how this can become a vicious cycle.11 12
Noise and light pollution
Besides being a source of frustration, environmental noise (particularly noise “caused by transportation means”) when you’re trying to sleep can actually have a negative impact on your overall health — even if you do manage to sleep through it.13 Peter James, an assistant professor of environmental health at Harvard University's T.H. Chan School of Public Health, explains that noise pollution can trigger the body’s fight-or-flight response, flooding the body with stress hormones.14 This can have a negative impact on sleep because, as mentioned above, increased stress makes it difficult to get good sleep.9
Similarly, light pollution has been linked to increased neuroinflammation, circadian rhythm disruptions, and detrimental effects on mental health, including the exacerbation of pre-existing mood disorders.15
With this information in mind, let’s take a look at the most (and least) sleep-deprived major cities in the United States.
The top ten most sleep-deprived major cities
While insufficient sleep is a nationwide problem, the eastern half of the United States seems particularly sleep deprived. Based on the results of our data analysis, the top ten most sleep-deprived cities are:
- Norfolk, Virginia
- New Orleans, Louisiana
- Detroit, Michigan
- Toledo, Ohio
- Cincinnati, Ohio
- Indianapolis, Indiana
- Philadelphia, Pennsylvania
- Laredo, Texas
- Cleveland, Ohio
- Memphis, Tennessee
As you may have noticed, Ohio is the only state on the above list that appears multiple times. (And it makes one more appearance in the top 20, with Columbus coming in at 14th place.) We’ll delve into more details later, but several of those Ohio cities also ranked high for various factors leading to poor sleep quality.
Pivoting to the other entries on the top ten list, the only city that isn’t in the eastern part of the country is Laredo, Texas. However, it’s worth pointing out that there are Midwestern and West Coast cities that also ended up pretty high in our rankings, including:
- Corpus Christi, Texas (11th)
- Las Vegas, Nevada (14th)
- North Las Vegas, Nevada (17th)
- San Antonio, Texas (19th)
- Honolulu, Hawaii (20th)
The top ten least sleep-deprived cities
As mentioned above, sleep deprivation is definitely a national problem, with clear room for improvement in every major metro area. But some interesting patterns did emerge from our data analysis. While most of the top sleep-deprived cities are in the eastern half of the country, the ten least sleep-deprived ones are mainly in the Midwest and the West, including:
- Minneapolis, Minnesota
- Seattle, Washington
- San Jose, California
- Madison, Wisconsin
- Boise, Idaho
- St. Paul, Minnesota
- Denver, Colorado
- Lincoln, Nebraska
- Oakland, California
- San Francisco, California
On this list, two states make multiple appearances: California (three times) and Minnesota (twice). Also worth mentioning is the fact that most of these cities are situated in areas with below-average nighttime temperatures. Some experts suggest that cooler temperatures can improve sleep, so that very well may be a factor at play.16
Though Midwestern and Western cities dominated the list of the ten least sleep-deprived cities, some Eastern cities rank quite well for sleep, such as:
- Raleigh, North Carolina (14th least sleep-deprived)
- Washington, District of Columbia (19th least sleep-deprived)
- Winston-Salem, North Carolina (24th least sleep-deprived)
- Durham, North Carolina (27th least sleep-deprived)
In the following section, we’ll explore the cities with the lowest sleep duration and worst sleep quality in more detail, including some interesting data points we noticed during our analysis.
Which cities have the worst sleep duration and quality?
As mentioned earlier, we evaluated each city’s sleep deprivation ranking based on citizens’ average sleep duration and the prevalence of five metrics — physical activity, obesity, alcohol consumption, mental distress, and noise and light pollution — that can impact sleep quality.
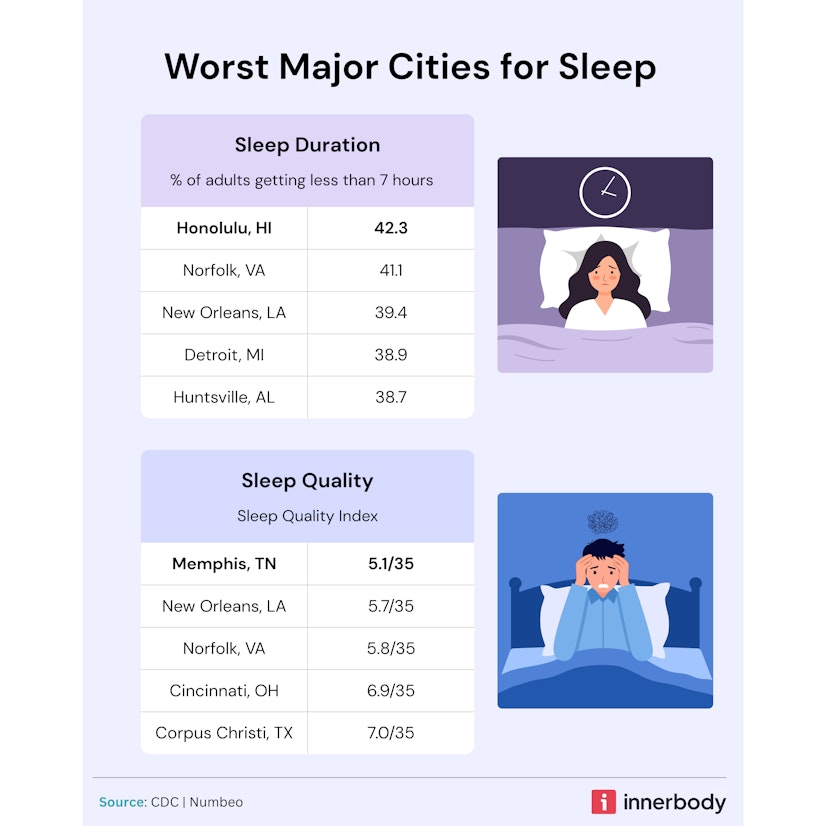
The cities with the shortest sleep duration
According to our analysis of CDC data, the cities with the shortest sleep duration include:
- Honolulu, Hawaii
- Norfolk, Virginia
- New Orleans, Louisiana
- Detroit, Michigan
- Huntsville, Alabama
Three of these cities also made it onto the top ten list of the most sleep-deprived cities: Norfolk, Virginia (1st), New Orleans, Louisiana (2nd), and Detroit, Michigan (3rd). The other two cities, Honolulu, Hawaii, and Huntsville, Alabama, also ranked fairly high for overall sleep deprivation, each earning a spot in the top 20. However, this list is the only time in which these two cities make an appearance in a top spot.
The cities getting the worst-quality sleep
The five cities getting the worst-quality sleep, according to our data, are:
- Memphis, Tennessee
- New Orleans, Louisiana
- Norfolk, Virginia
- Cincinnati, Ohio
- Corpus Christi, Texas
Again, New Orleans, Louisiana, and Norfolk, Virginia, are high-ranking. But you may also notice that two other cities from the top ten most sleep-deprived cities list made this one, too: Memphis, Tennessee (10th), and Cincinnati, Ohio (5th). The only entry in the above list that didn’t make the top ten is Corpus Christi, Texas, but it’s not too surprising to see, given that it ranked 11th most sleep-deprived.
If you’re curious about the top five cities for each individual sleep quality metric, the rankings are as follows. (Note: those that also made the top ten most sleep-deprived list are marked with the associated ranking.)
Top five least physically active in leisure time:
- Laredo, Texas (8th)
- Corpus Christi, Texas
- El Paso, Texas
- Memphis, Tennessee (10th)
- Miami, Florida
Top five with the highest obesity rates:
- Corpus Christi, Texas
- Memphis, Tennessee (10th)
- Laredo, Texas (8th)
- Toledo, Ohio (4th)
- Chesapeake, Virginia
Top five highest rates of mental distress:
- Memphis, Tennessee (10th)
- Toledo, Ohio (4th)
- Norfolk, Virginia (1st)
- New Orleans, Louisiana (2nd)
- Richmond, Virginia
Top five for binge drinking:
- Denver, Colorado
- Washington, District of Columbia
- Madison, Wisconsin
- San Francisco, California
- Minneapolis, Minnesota
Top five for noise and light pollution:
- Newark, New Jersey
- Anaheim, California
- Memphis, Tennessee (10th)
- New York, New York
- Norfolk, Virginia (1st)
It’s interesting that multiple cities from the ten least sleep-deprived list appear on the top five list for prevalence of binge drinking: Denver, Colorado (7th), Madison, Wisconsin (4th), San Francisco, California (10th), and Minneapolis, Minnesota (1st). This is the only instance in which any of the least sleep-deprived cities ranked high for a factor with a negative impact on sleep quality. But it is just one of the five factors contributing to the picture of sleep quality; their relatively low prevalence of mental distress and obesity, alongside strong sleep duration scores, buoyed these cities in our assessment.
The full rankings
Though we’ve covered quite a few cities across the country, you may be curious if and where yours ended up on the list (if it hasn’t already been mentioned). The sortable table below breaks down the rankings of all 100 major cities we evaluated, overall rank of 1 being the most sleep-deprived city and 100 being the least sleep-deprived city. In all columns that follow the total population rank, a rank of 1 indicates the highest prevalence, while rank 100 indicates lowest prevalence.
How to get more deep sleep
Whether or not your city made it onto this list, you may be looking for solutions on how to sleep better — a valuable pursuit. In the following sections, we’ll cover some methods you can use to try to improve your own sleep hygiene and achieve some quality rest.
Regular exercise
Exercise can have a major positive impact on sleep, from promoting the production of melatonin to reducing stress, improving your mood, and more.3
But you don’t have to hit the gym every day to achieve this. A 2024 study found that participants who exercised “at least two or more times a week, for 1 hour/week or more” experienced better sleep.21 So even taking a 30-minute walk twice a week could help you reap these benefits.
Reduce electronics use before bed
The artificial blue light emitted from electronic devices — smartphones, laptops, etc. — can alter your brain’s production of melatonin and negatively impact your circadian rhythms. To prevent this impact, it’s recommended that you avoid blue light exposure for 2-3 hours before bedtime.22
Try going to bed earlier
Most healthy adults over the age of 18 need seven or more hours of sleep per night, and those who get less may experience more frequent health concerns.23 24 So, though it may not seem like a big difference, five or six hours of sleep is not enough. But an earlier bedtime may help you get that extra hour or two and improve your long-term physical and mental health.
This is supported by a few different pieces of research. According to the findings of a 2020 review, “earlier sleep timing and regularity in sleep patterns with consistent bedtimes and wake-up times” can lead to better health outcomes.25 And a 2024 study found that “night owl” behaviors (a preference for staying up late and waking up late) increased participants’ risk of being diagnosed with a mental health disorder. In comparison, those with “morning lark” behaviors (going to sleep early and getting up early) had the best mental health outcomes. It’s worth mentioning that the study’s authors point out that night owls who followed a morning lark routine, despite their preferences, fared better than night owls who stuck with a later schedule.26
Sleep aids
Though studies have shown positive results from using melatonin for sleep, it’s far from the only effective over-the-counter sleep aid available.17 Products like CBD, CBN gummies, and magnesium supplements all have demonstrated efficacy in studies.
For example, CBD appears to be beneficial for those with sleep apnea and narcolepsy,18 CBN isolate may reduce nighttime wakefulness,19 and individuals with a higher magnesium intake may experience better sleep quality.20
Methodology
For this study, we started with the top 100 U.S. cities by population. From there, we analyzed relevant metrics from three large data sets:
- The CDC's Behavioral Risk Factor Surveillance System (BRFSS), which is survey data of adults 18 and older and defines short sleep duration as anything less than seven hours of sleep.
- Data sets from the CDC's PLACES 2024 data release
- Numbeo’s noise and light pollution index data for cities
We created a ranking system to determine how the major U.S. cities ranked for sleep deprivation. Our ranking system weights the prevalence of short sleep duration at 65% (source: CDC) and combines that with our sleep quality index weighted at 35%. Our sleep quality index is determined by a combination of the following five data factors, all of which are sourced from the CDC except where noted:
- Prevalence of obesity
- Prevalence of no leisure-time physical activity
- Prevalence of frequent mental distress
- Prevalence of binge drinking
- Noise and light pollution (source: Numbeo)
These five factors are significant contributors to poor sleep quality. We weighted mental distress and obesity higher than leisure-time physical activity as sleep quality factors since many workplaces also involve physical activity.
Fair use statement
Innerbody Research is committed to providing objective, science-based suggestions and research to help our readers make more informed decisions regarding health and wellness. We invested the time and effort into creating this report to explore which U.S. states are suffering the most from sleep deprivation. We hope to reach as many people as possible by making this information widely available. As such, please feel free to share our content for educational, editorial, or discussion purposes. We only ask that you link back to this page and credit the author as Innerbody.com.
Sources
Innerbody uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
Adjaye-Gbewonyo, D., Ng, A., & Black, L. (2022). Sleep Difficulties in Adults: United States, 2020. CDC.
National Institutes of Health. (2022). What Are Sleep Deprivation and Deficiency? National Heart, Lung, and Blood Institute.
Alnawwar, M. A., Alraddadi, M. I., Algethmi, R. A., Salem, G. A., Salem, M. A., & Alharbi, A. A. (2023). The Effect of Physical Activity on Sleep Quality and Sleep Disorder: A Systematic Review. Cureus, 15(8), e43595.
Jehan, S., Zizi, F., Pandi-Perumal, S. R., Wall, S., Auguste, E., Myers, A. K., Jean-Louis, G., & McFarlane, S. I. (2017). Obstructive Sleep Apnea and Obesity: Implications for Public Health. Sleep Medicine and Disorders: International Journal, 1(4), 00019.
Cleveland Clinic. (2025). Sleep Apnea. Cleveland Clinic.
Yale Medicine. (2023). The Connection Between Sleep, Diabetes, and Obesity. Yale Medicine.
Park, Y., Oh, K., Lee, S., Kim, G., Lee, J., Lee, H., Lim, T., & Kim, Y. (2015). The Effects of Alcohol on Quality of Sleep. Korean Journal of Family Medicine, 36(6), 294.
Simou, E., Britton, J., & Leonardi-Bee, J. (2018). Alcohol and the risk of sleep apnoea: A systematic review and meta-analysis. Sleep Medicine, 42, 38.
Harvard Medical School. (2021). Sleep and Mood. Harvard Medical School: Division of Sleep Medicine.
Neckelmann, D., Mykletun, A., & Dahl, A. A. (2007). Chronic Insomnia as a Risk Factor for Developing Anxiety and Depression. Sleep, 30(7), 873.
Staner, L. (2003). Sleep and anxiety disorders. Dialogues in Clinical Neuroscience, 5(3), 249.
Johns Hopkins Medicine. (n.d.). Depression and Sleep: Understanding the Connection. The Johns Hopkins University.
Halperin, D. (2014). Environmental noise and sleep disturbances: A threat to health? Sleep Science, 7(4), 209.
Harvard Chan Staff Writer. (2023). Noise pollution can lead to sleep issues, chronic health problems. Harvard T.H. Chan School of Public Health.
Menculini, G., Cirimbilli, F., Raspa, V., Scopetta, F., Cinesi, G., Chieppa, A. G., Cuzzucoli, L., Moretti, P., Balducci, P. M., Attademo, L., Bernardini, F., Erfurth, A., Sachs, G., & Tortorella, A. (2024). Insights into the Effect of Light Pollution on Mental Health: Focus on Affective Disorders—A Narrative Review. Brain Sciences, 14(8), 802.
Rabago, N. (2023). A cold room, not a warm bath, encourages sleep. The University of Texas Health Science Center at San Antonio.
Costello, R. B., Lentino, C. V., Boyd, C. C., Crawford, C. C., Sprengel, M. L., & Deuster, P. A. (2014). The effectiveness of melatonin for promoting healthy sleep: A rapid evidence assessment of the literature. Nutrition Journal, 13, 106.
Babson, K. A., Sottile, J., & Morabito, D. (2017). Cannabis, cannabinoids, and sleep: A review of the literature. Current Psychiatry Reports, 19(23).
Bonn-Miller, M. O., Feldner, M. T., Bynion, T. M., Eglit, G. M. L., Brunstetter, M., Kalaba, M., Zvorsky, I., Peters, E. N., & Hennesy, M. (2024). A double-blind, randomized, placebo-controlled study of the safety and effects of CBN with and without CBD on sleep quality. Experimental and Clinical Psychopharmacology, 32(3), 277-284.
Zhang, Y., Chen, C., Lu, L., Knutson, K. L., Carnethon, M. R., Fly, A. D., Luo, J., Haas, D. M., Shikany, J. M., & Kahe, K. (2021). Association of magnesium intake with sleep duration and sleep quality: Findings from the CARDIA study. Sleep, 45(4), zsab276.
Bjornsdottir, E., Thorarinsdottir, E. H., Lindberg, E., Benediktsdottir, B., Franklin, K., Jarvis, D., Demoly, P., Perret, J. L., Aymerich, J. G., Dorado-Arenas, S., Heinrich, J., Torén, K., Larsen, V. G., Jögi, R., Gislason, T., & Janson, C. (2024). Association between physical activity over a 10-year period and current insomnia symptoms, sleep duration and daytime sleepiness: A European population-based study. BMJ Open, 14(3), e067197.
Harvard Medical School. (2024). What is blue light? The effect blue light has on your sleep and more. Harvard Health Publishing.
Olson, E. (2025). How many hours of sleep are enough for good health? Mayo Clinic.
National Institutes of Health. (2022). How Much Sleep Is Enough? National Heart, Lung, and Blood Institute.
Chaput, J. P., Dutil, C., Featherstone, R., Ross, R., Giangregorio, L., Saunders, T. J., Janssen, I., Poitras, V. J., Kho, M. E., Ross-White, A., Zankar, S., & Carrier, J. (2020). Sleep timing, sleep consistency, and health in adults: a systematic review. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme, 45(10 (Suppl. 2)), S232–S247.
Lok, R., Weed, L., Winer, J., & Zeitzer, J. M. (2024). Perils of the nighttime: Impact of behavioral timing and preference on mental health in 73,888 community-dwelling adults. Psychiatry Research, 337, 115956.


